- About
- Research
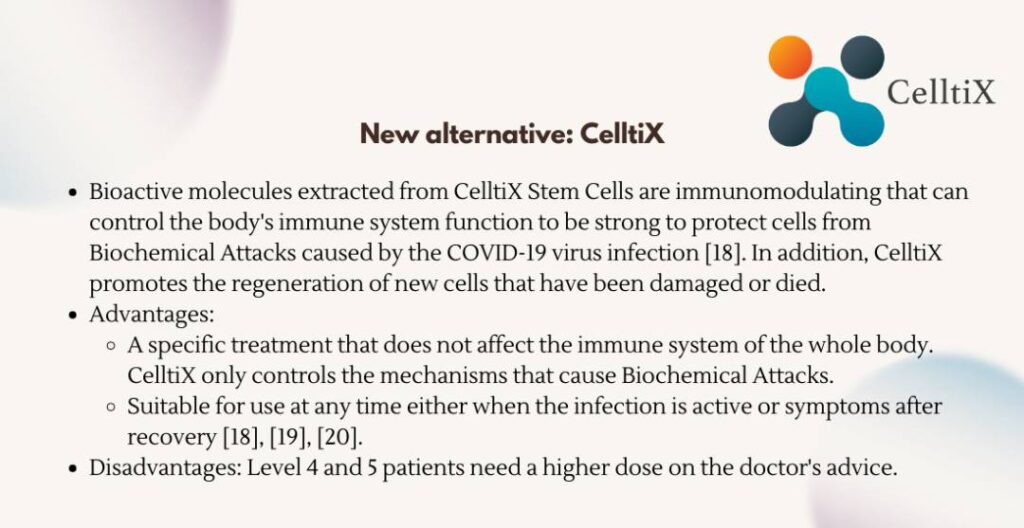
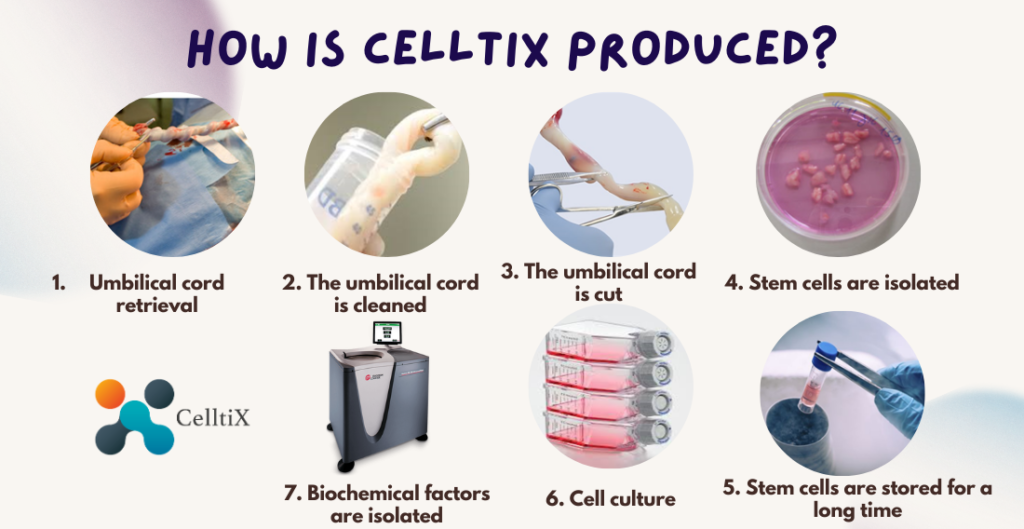
- Product
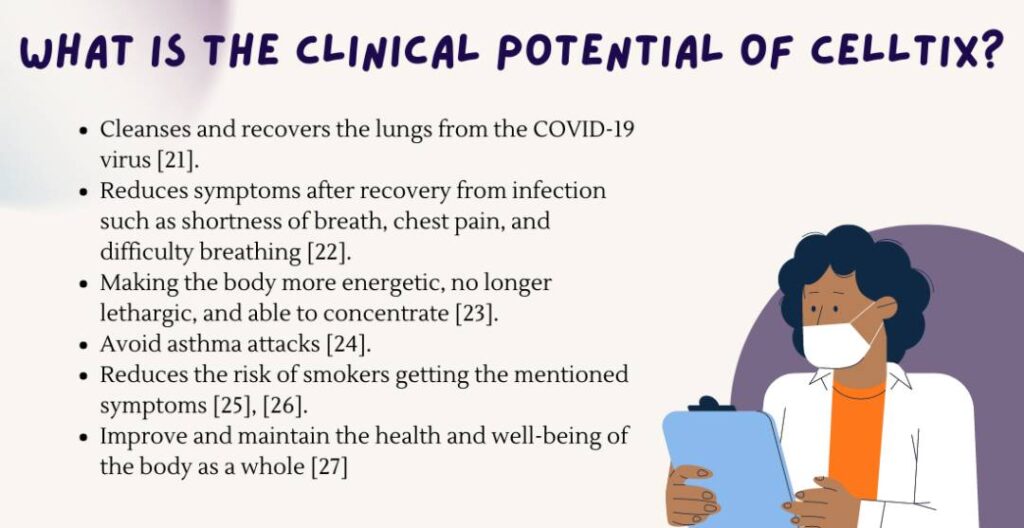
- Medical Use
- CelltiX Nebulizer
- HOME
- ABOUT
- RESEARCH
- INSIGHTS & HAPPENINGS
- JOIN US
- CONTACT US
-













Established in 2010, Cell Tissue is a Malaysian advanced medical technologybased company, a spin-off of the National University of Malaysia (UKM), one of the country’s leading universities and research institutes.
Cell Tissue is known as Malaysia’s FIRST Tissue Engineering Firm, awarded by the prestigious Malaysian Book of Records in 2016, operated in a certified Current Good Manufacturing Practice (cGMP) laboratory following PIC/S standards by the National Pharmaceutical Regulatory Agency (NPRA), a division of the Ministry of Health Malaysia.

Proudly powered by CTTSB © 2010-2024 Cell Tissue Technology Sdn Bhd, a Universiti Kebangsaan Malaysia spin-off Company. – All rights reserved.